What materials exist, and how do they compare?
Before implant restoration became widespread, Guided Tissue Regeneration (GTR) procedures were offered, which utilised dental membranes to exclude gingival tissue from occupying a periodontal pocket, giving periodontal tissues the space and time to regenerate. The first barrier membranes (expanded ptfe AKA GoreTex) created the required healing compartment, yet required a second procedure to remove. These materials were associated with a high incidence of dehiscence and infection, prompting the development of a bioresorbable matrix barrier by Gottlow and co-workers in the late 1980s.
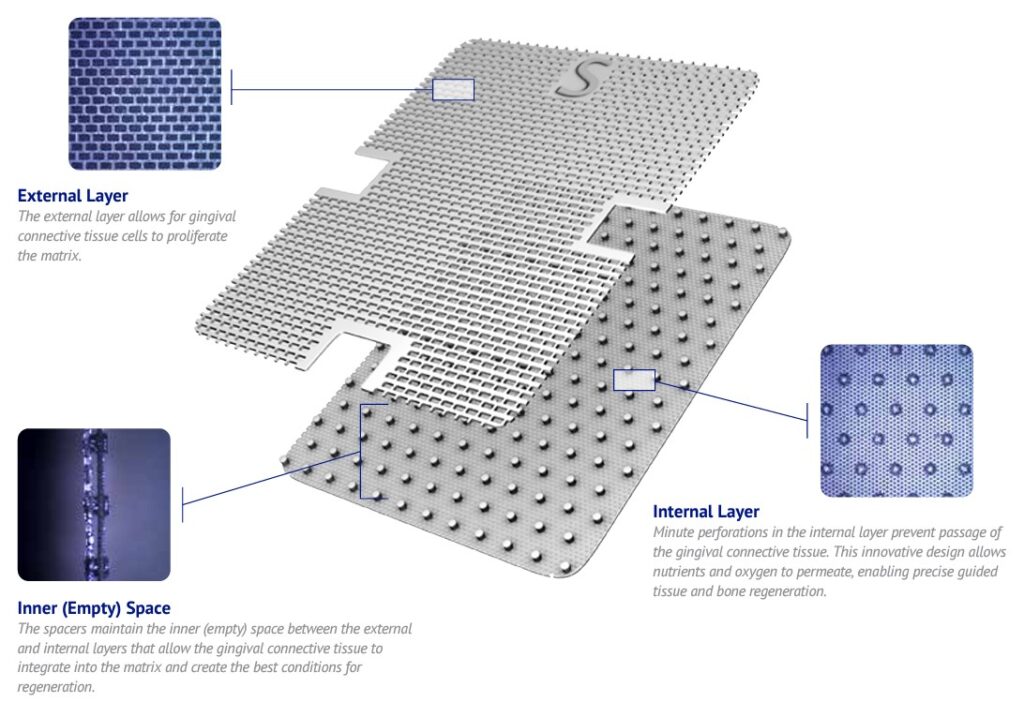
Image shown:
Guidor bioresorbable matrix barrier
Guided Bone Regeneration (GBR)
As Dental Implant use increased, the materials used for GTR were revised to meet the needs of GBR, with resorbing collagen appealing to the emerging GDP community.
One of the challenges when using collagen membranes is the collapse into the defect, which led to the emergence of proprietary bone void fillers in combination with barrier membranes.
WHEN IS A BARRIER MEMBRANE NEEDED?
Today, more advanced proprietary bone graft materials exist which deliver excellent new bone without a dental membrane. One example is Powerbone Dental Putty.
When indicated, a Barrier Membrane carries three key functions:
WHAT TYPE OF BIORESORBING DENTAL MEMBRANES EXIST TODAY?
Fully resorbing dental barrier membranes can be distinguished by their origin and the time frame in which the barrier function is maintained. Two types exist: those of animal origin nd those produced in the laboratory from various polymers.
Animal origin – Collagen Membranes.

Collagen is a protein that makes up the structure or framework in connective tissue, skin, tendons, bones, and cartilage. The collagen used in resorbable dental membranes is sourced from the pericardial or peritoneal areas of pigs or cows. Pericardial collagen presents a higher mechanical strength than peritoneal collagen.
The first bovine peritoneal collagen (Geistlich Bio-Gide) is less stiff and more prone to collapse into the wound, promoting the development of extended-function collagen materials.
Functional resorption time is different from complete resorption time, as non-functional remnants will remain long after the intended barrier function is compromised. Because native collagen is a protein, it can resorb quickly. If exposed to saliva, this dissolution can be rapid. Quick resorption impacts function and is a limiting factor for the use of native collagen membranes in dental bone graft procedures and is the main reason Geistlich recommends two layers for its Bio-Gide.
Animal origin – Cross-linked Collagen.
Methods to extend the resorption time of collagen membranes include chemical and physical processing. Processing with chemicals such as glutaraldehyde successfully extends the resorption time for a collagen membrane. Some products cross-linked with high concentrations of glutaraldehyde show an increased inflammatory response.
Cross-linking Collagen via process development.
For these reasons, methods to physically modify the collagen were developed, such as dehydrothermal (DHT) treatment. When applied to porcine pericardial-sourced collagen, DHT treatment produces a membrane that exhibits high tensile strength, resistance to degradation, with reduced inflammatory responses. The handling characteristics of cross-linked collagen can differ, with some materials stiffer than others. This can have advantages and disadvantages. An example of softer, more pliable material is T-Gen, whilst Ti-oss Guide is stiffer and presents a greater space creation effect.
Laboratory origin – Polymer Membranes
The polymer materials of polylactic (PLA), polyglycolic (PGA), and poly(lactic-co-glycolic) acid (PLGA) are widely used in various medical applications, e.g. as resorbable implants in surgery, as raw materials for wound closure stitches or as carrier substances for the delivery of pharmaceuticals. They present excellent biocompatibility and adjustable degradation rate and are non-toxic in humans. (1) and were the first resorbable materials used for GTR and GBR with high tensile strength and excellent space maintenance.
HANDLING.
One or two-layer Polymer Membranes.
Clinicians familiar with PTFE will find the double-layer Powerbone Resorbing Synthetic familiar. Clinicians transitioning from Resorbable Collagen, such as Ti-oss Guide, should consider the single-layer Powerbone Resorbing Synthetic version more familiar.
Thermo-mouldable membranes aid conformity.
Resorbable polymer membranes such as Powerbone Polymer Membrane can be thermo moulded before application, making them more able to match the bone architecture. When used in this way, resorbing polymer membranes create better space and are more substantial barriers than resorbing collagen. Warming is done by placing the final packaging into hot water before placement. Fixation is mandatory to ensure defect continuity.
FIXATION.
A dental barrier membrane must be stable and be in contact with healthy surrounding bone. For this reason, fixation is recommended.


Fixation is with membrane tacks that are available in titanium or produced from a resorbable polymer.
Both are produced with barbs or ridges on their side to grip the bone and are pushed into place using a holding tool. Some GBR and Fixation kits include a pilot drill to create a small osteotomy to aid grip.
BROWSE AND PURCHASE
Resorbable and non-resorbable membranes and fixation tools can be browsed and purchased online from Regen store HERE.
References