Can socket preservation be completed predictably without the additional surgical complications of flap creation, membrane application and tension-free closure?
Studies show socket grafting with biomaterials prevents atrophy.
Different biomaterials (autogenous, allogenic, synthetics, xenografts) and biological preparations (PRF, PRP, PRGF) are proposed to fill the extraction sockets with multiple protocols followed to achieve this. Irrespective of origin, the processing of biomaterials affects their resorption characteristics which in turn impacts the level of bone regeneration and space maintenance achieved. A fully resorbing bone graft will generate more bone and is ideal when an implant is scheduled. A slow-resorbing biomaterial will favour volume preservation and is more suitable when an implant-supported restoration is not scheduled as it will be more resilient to natural remodelling and atrophy. You can read more about this below and in our ‘tooth out what next’ article.
Conventional wisdom – primary closure
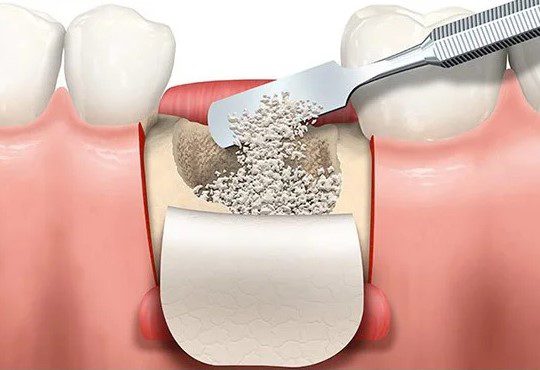
Conventional techniques for ridge preservation with socket grafting involve primary closure where a buccal full-thickness flap is raised and advanced to cover and protect the socket and dental membrane. Achieving primary closure prolongs surgical time and complexity, increases morbidity and delays healing.
Typical Dental Membranes are COLLAGEN, which adds cost and complexity. Collagen membranes require complete tissue coverage because, as a protein, salivary enzymes will quickly dissolve them. Alternatives to collagen are POLYMER MEMBRANES such as PTFE or Powerbone Polymer membrane. PTFE will require a 2nd procedure for removal whereas Powerbone Polymer membrane adsorbs fully negating the removal procedure.
Aesthetic implications.
In addition, raising and advancing a flap to cover the extraction socket and create space to secure the dental membrane results in the disturbance of the vestibule buccally and the loss of the buccal keratinized soft tissues. This compromises aesthetic and functional results which may require additional surgical interventions to overcome.
Grafts designed for open healing sites.
Particulate or granular grafts are mobile and require the protection and support of a barrier membrane with corresponding flap management compromises. (see below)

In the last decade, several bone grafting technologies have emerged that match the morphology of the site and offer self-stabilising features removing the need for a barrier membrane.
These technologies are differentiated by their format (Dental Putty, Cement, Sponge Cone) and their respective resorption profiles (Full or partial).
The decision about the resorption profile of the bone graft chosen should be taken based on the restorative plan – IMPLANT YES or IMPLANT NO.
| IMPLANT YES? | IMPLANT NO? |
| A fully resorbing material generates maximum new bone volume in the shortest time. | A partially resorbing material will preserve the volume for longer at the expense of less new bone. |
| Powerbone Dental Putty is a fully synthetic material applied directly from its syringe. It compresses to match the socket and is self-stabilising. Powerbone Dental Putty will regenerate up to 50% new bone within 12 to 14 weeks. | Biphasic Socket Cone Graft contains a fully synthetic biphasic calcium phosphate. It compresses to match the socket shape and is self-stabilising. The HA component of the biphasic is more resilient to remodelling and ensures longer-term volume preservation. |
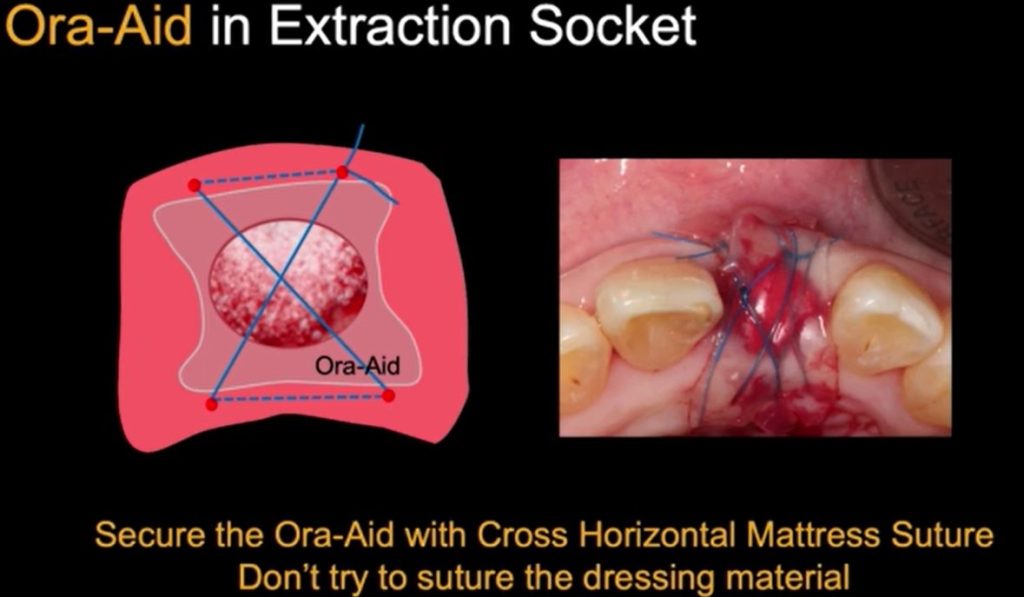
Both Powerbone Dental Putty and Biphasic Cone Graft are form-stable and will not move around. For both, we recommend protecting the site with an Ora-Aid self-sealing dressing to encourage soft tissue healing by secondary intention. Ora-Aid can be held in place for a longer period with a cross suture slung over but not through the dressing or a tissue glue. This is further described below.
Healing without Primary Closure.
Ridge preservation, the placement of a bone graft, and maintenance of optimal aesthetics can be successfully achieved without primary closure. The main advantage of not obtaining primary closure is an increased area of keratinized gingiva and stable mucogingival junction as well as less trauma and surgical time.

Numerous studies utilising form-stable calcium phosphate technologies show complete coverage by newly formed keratinized tissue at 12 weeks with maintenance of ridge volume and architecture. A flap is not advanced to cover the exposed graft in such cases. Instead, the site is protected topically to reduce graft loss in the first few days.
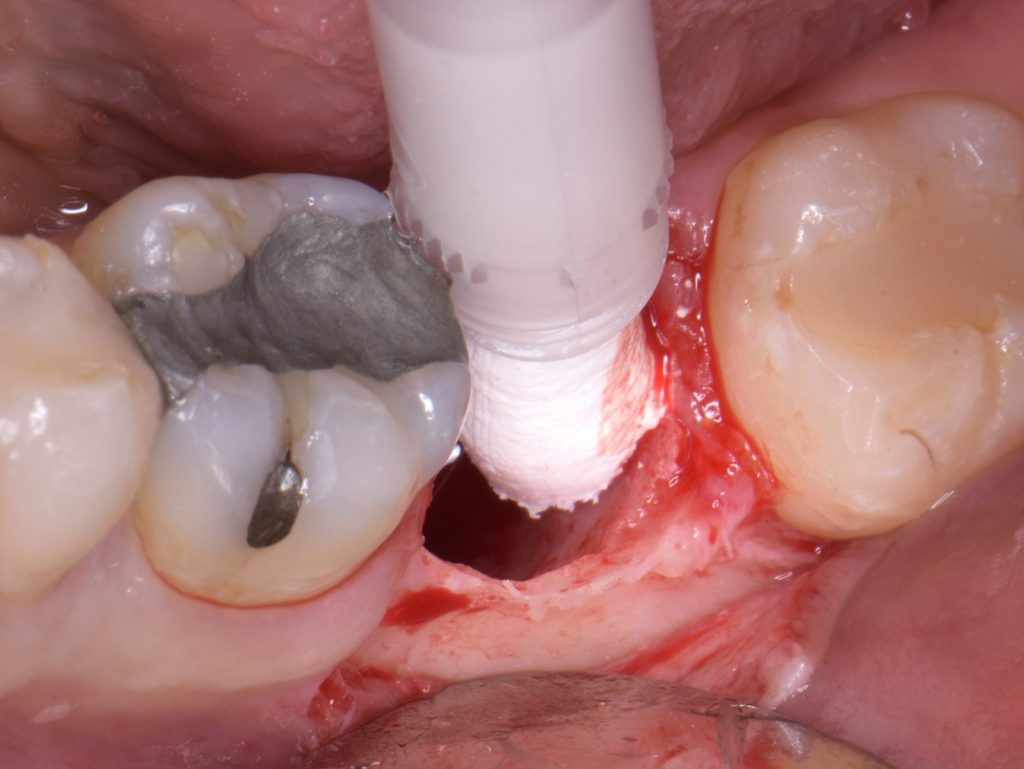
Powerbone Dental Putty -Clinical Protocol
The protocol for open healing grafting using Powerbone Dental Putty is beautifully illustrated in a compelling presentation by Dr Minas Leventis shown HERE.
Graft Protection
Graft protection is especially critical in molar sites where the larger size of the socket requires a much longer time for soft tissue healing and complete coverage of the graft, compared to smaller anterior extraction sites. A variety of materials are proposed to be suitable in such cases.

DENSE COLLAGEN SPONGE – A Parasorb cone can be compressed between the fingers and placed over the site to provide short-term sacrificial protection. Retention with a cross suture is recommended.
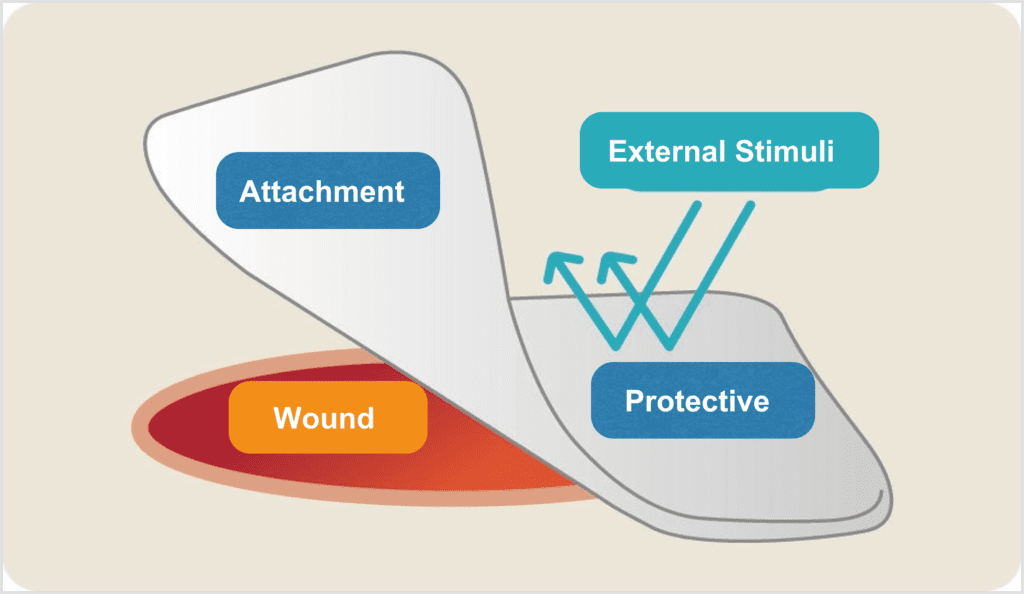
ORA-AID – Ora-Aid is a novel self-sealing barrier that protects the site allowing open healing ridge preservation and protection of grafts and other materials placed inside the socket. Ora Aid is available in two sizes – 25 x 15mm and 50 x 15mm. When exposed to saliva and blood the Ora-Aid lower layer becomes adhesive whilst the upper layer creates a smooth protective surface due to the inclusion of a water-insoluble polymer with a mint flavour.

PERIACRYL TISSUE ADHESIVE – PeriAcryl 90 HV is a combination perfect for perio, implant and oral surgery. The HV formulation is 9 times thicker than the original, which helps with application. A violet colour aids visualisation. PeriAcryl 90 HV will stay in place for approximately 7-10 days and slough off naturally as the healing occurs underneath.
Both Ora-Aid and PeeriAcryl HV adhesive seal the wound from pathogens and accelerate healing.
Secure Suture or Tissue Adhesive
A combination of Ora-Aid with a cross suture prolongs the application time of Ora-Aid. We recommend Polyglactin 910 multifilament (Vicryl type) or the newer adsorbing Monofilament PGCL as a sling over, but not through the Ora-Aid. An alternative is to secure the site with PeriAcryl tissue adhesive.
For further information, ask@regen-store.co.uk
Clinical images courtesy of Dr Minas Leventis (UK) and Dr Marcelo Faveri (Brazil)
References: